Medical Billing and Forwarding
Medical Forwarding: The process of Forwarding medical bill to Insurance company.
Medical Billing:The process of submitting and following up on claims with health insurance companies in order to receive payment for services rendered by a healthcare provider. The same process is used for most insurance companies, whether they are private companies or government sponsored programs.
SIDSOFT Medical Billing and Forwarding
Does your medical facility want to focus on core medical functions, minimize billing denials, increase efficiency in the billing process, cut down on costs, and ensure timely reimbursement all at the same time?
medical billing and coding to skilled offshore service providers like all the above mentioned benefits without any hassles. As our customer, your medical facility can get access to quality medical coding and billing, while reducing your current operating costs by at least 40%. Our end-to-end medical billing and coding solutions can meet all your needs, from following up on pending medical claims, to getting reasons for denied claims, tracking receivable balances, or initiating collections.
Stages of Medical Billing
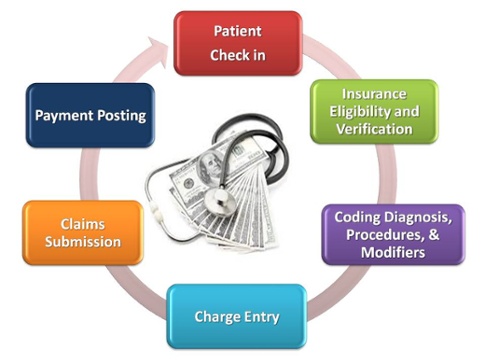
- Patient Check-in:
The very first stage of a patient's appointment should include the notation of the patient's demographic information as well as information about his/her insurance, such as the insurance payer and policy number. Any information that will be useful and/or necessary in a claim situation should be detailed at patient check-in.
- Insurance Eligibility and verification:
Even regular patients need to verify their insurance information and eligibility before every appointment. Insurance information can change at any time, which is why you need to ask patients before every visit if their insurance information has changed. A change in insurance information can also impact benefit and authorization information, so it is always worth the trouble of double-checking.
- Coding of Diagnosis, Procedures and Modifiers:
The correct coding of claims is vital for informing the insurance payer of what exactly the patient is being treated for as well as the method of treatment the patient is undergoing. Be sure to use the correct diagnosis codes to describe the patient's symptoms or illnesses and the correct procedure codes to describe the patient's method of treatment. Use accurate CPT and HCPCS code modifiers to provide additional information about the service or procedure performed. The insurance payer can only make an accurate assessment if they have the correct codes and modifiers.
- Charge Entry:
This refers to entering the charges for services that the patient received. The charge entry also includes the appropriate linking of medical codes to services and procedures rendered during the patient's visit.
- Claims Submission:
Once the claim has been properly completed, it must be submitted to the insurance payer for payment. Medical billers need to have access to the information they need about the insurance payer since there are so many variables for each insurance payer in determining how and when to submit a claim. While most insurance companies follow a standard set of guidelines for billing, there are some payers who have a separate way of doing things. Certain aspects of medical billing are payer-specific, so it is important to check with each payer to make sure you are accurately following their guidelines for claims submission.
- Payment Posting:
This last step involves posting and deposit functions. At this point, the amount billed to the patient will be zero if it has been paid in full or it will reflect the amount owed by the patient. The insurance payer's responsibility should have been met by this step in the process.
Package System
Packages are in fashion today for most surgical procedures in various corporate hospitals and this has included laparoscopic procedures too. A package system enables the hospitals to get cost settlements done more easily. Also, it is more convenient for the patients who are aware upfront of the charges.
A package is defined as a lump sum cost of inpatient treatment for which a patient has been referred by a competent authority or CGHS to the hospital or diagnostic center. This includes all the charges pertaining to a particular treatment/procedure including registration charges, admission charges, accommodation charges, injection/transfusion charges, dressing charges, operation charges, anesthetic charges, operation theatre charges, procedural charges/surgeon fee, doctor/consultant visit charges, ICU/ICCU charges, monitoring charges, cost of disposable surgical charges and cost of all sundries used during hospitalization-related routine investigation, and physiotherapy charges, etc. from the time of admission to the time of discharge
Advantages of the package system
- The package system was forced upon the hospitals by various government establishments and insurance companies when it was realized that there is a great variation in the cost of laparoscopic surgery in different hospitals in various corners of the country. A laparoscopic cholecystectomy at smaller nursing homes may cost around Rs. 10 000, which may be double if performed at large private hospitals
- The package system ensures uniformity of surgical expenses, less inconvenience for the patient and the company′s approval for the surgery. It is time to question as to how the packages are fixed. A few bureaucrats and doctors, based on the basic salary of the patient or his dependent, decide as to what package he is entitled to in the general/special ward. In most of the cases, the packages are faxed to the concerned employee and the money for the surgical expenses is sanctioned even before the surgeon has wheeled in the patient to the operation theatre.
Types of Medical Billing
They are two types of Medical Billing:
- Professional Billing
Professional billing is responsible for the billing of claims generated for work performed by physicians, suppliers and other non-institutional providers for both outpatient and inpatient services. Professional charges are billed on a CMS-1500 form. The CMS-1500 is the red-ink on white paper standard claim form used by physicians and suppliers for claim billing.
- Institutional Billing
Institutional billing is responsible for the billing of claims generated for work performed by hospitals, skilled nursing facilities, and other institutions for outpatient and inpatient services including the use of equipment and supplies, laboratory services, radiology services, and other charges. Institutional charges are billed on a UB-04. The UB-04 is the red-ink on white paper standard claim form used by institutional providers for claim billing.
Componets of Billing
- Inpatient"Inpatient" means that the procedure requires the patient to be admitted to the hospital, primarily so that he or she can be closely monitored during the procedure and afterwards, during recovery.
Fee Structure to be included for Inpatient:
- Bed charges : A hospital bed or hospital cot is a bed specially designed for hospitalized patients or others in need of some form of health care
- Nursing Charges: Nursing Charges consists of the performance of the leadership functions of governance and decision-making within organizations employing nurses. It includes processes common to all management like planning, organizing, staffing, directing and controlling.
- Doctot visit Charges:Doctor visit charges varies from one hospital to another hospital
- OT charges:Ready to do extra work than fixed working hour
- Anesthesia Charges: Anaesthesia refers to the practice of administering medications either by injection or by inhalation (breathing in that block the feeling of pain and other sensations, or that produce a deep state of unconsciousness that eliminates all sensations, which allows medical and surgical procedures to be undertaken without causing undue distress or discomfort.
- Post Operative Care Charges: Postoperative care refers to the care you receive following a surgical procedure. This may include pain management and wound care.
- Drug Charges: Drug Chares Certain illicit drugs, such as cocaine and methamphetamine, are restricted at both the federal and state level. This includes the manufacturing, cultivation, trafficking, distribution and possession of these substances.
- Lab testing Charges: Lab testing Charges are medical procedures that involve testing samples of blood, urine, or other tissues or substances in the body.
Different kinds of charges
- Direct Payment:The Direct Pay Price is the maximum price that a patient would pay for the standard treatments for the specified diagnoses/services regardless of insurance status, if paid directly by the patient or the patient’s employer.
- Insurance Claim : A formal request to an insurance company asking for a payment based on the terms of the insurance policy. Insurance claims are reviewed by the company for their validity and then paid out to the insured or requesting party (on behalf of the insured) once approved.
- Government claim:while paying Bill they will consider whether patient is senior citizen,Blind people.
- Reference claim: Through some of refernce Doctor they will pay the bill.
- Patient Registration: The collection of data about new patients to start generating a patient record.
- Outpatient"Outpatient" means that the procedure does not require hospital admission and may also be performed outside the premises of a hospital
Our Medical Billing & Forwarding Solutions
We offer an entire gamut of medical billing and Forwarding services that include:
Why Should Your Hospital or Healthcare Facility Billing ?
Here is why your hospital, clinic or multi-specialty group should consider medical billing and coding:
- Save on infrastructure-related (hardware and software) expenses
- Minimize your current billing and coding costs by a whopping 40-60%!
- No need to pay for employee benefits or employee absenteeism
- No billing and coding staff turnover
- Eliminate the need to train new resources
- Experience a drastic reduction in denials with accurate data management
- Get faster reimbursements with accurate processing and submission of claims
- Benefit from zero billing errors
- Get fewer denials with error-free claims
- Improved and steady cash flow
Why Choose SIDSOFT for Medical Billing Forwarding Services?
-
Drastic reduction in the number of denials: Flaws in coding or inaccuracies in data are the main causes for claims getting denied. With the skilled SIDSOFT billing and Forwarding team handling your claims, you will see a sharp reduction in the number of denials in just a few days.
-
Regular reports:
Our team will keep you updated about the status of your claims, by providing you with daily, weekly and monthly progress reports. The reports will include details about productivity, procedure code analysis, projections and pending problems, if any.
-
Process-driven approach:
We follow a process that includes steps such as Insurance Eligibility Verification, Patient Demographic Entry, Charge Entry, Claims Submission, Accounts Receivables Follow-up, Payment Posting , Denial Analysis and Accounts Receivables Management.
-
Customized solutions:
We are very flexible and can provide you with customized medical billing and Forwarding services to meet your specific requirements.
-
Medical billing and Forawarding or varied specialties:
we have expertise in working with multiple specialties, such as microbiology, ophthalmology, radiology, pulmonary, obstetrics and gynecology, neurology, anesthesiology, cardiology, critical care, endocrinology, emergency surgery, general surgery and gastroenterology, amongst others.