Charge Entry
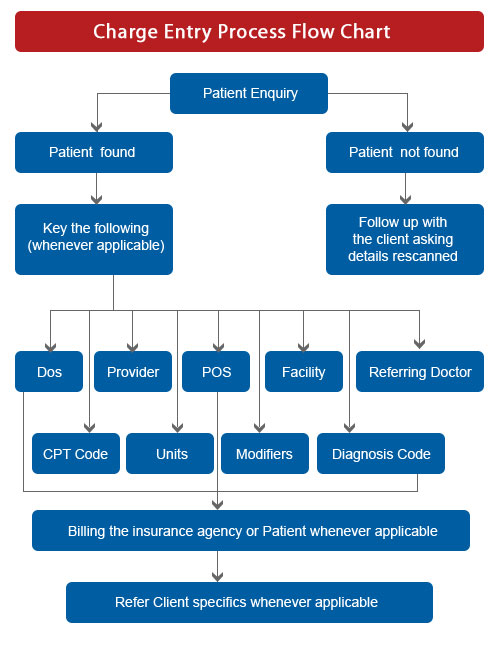
At SIDSOFT, we follow a well-structured charge entry process. The detailed steps followed through the process ensure that relevant checks are made at each processing stage. This enables us to manage a zero-error process and provide our services to you with speed and efficiency.
Our Billing Resources team has substantial experience and understanding of the US healthcare industry, and offers expert skills in facilitating investigations and enabling quality decision-making.
The Varied Steps We Manage Within Our Charge Entry Process are Described Below:
Step 1 - Receipt of Files
EOBs (Explanation of Benefits) and cheques are received from the client in a scanned format through our secure FTP site.
Step 2 - File Download and Allocation
Our Medical Billing team downloads the files received via the FTP site, reviews the material received and allocates processing work to the Payment Posting team.
Step 3 - Entry of Patient Demographics
The Payment Posting team captures a series of demographic data, which includes patient reference and billing system particulars such as patient account number, amount allowed, amount billed, amount adjusted and amount paid. Along with these, denial related details are also entered into the billing system.
Step 4 - EOB Follow Up
In cases where partial payments are made, necessary investigation and analysis is initiated, after which corrective steps are taken.
Step 5 - Denial Analysis
Flatworld's Billing Resources team conducts an investigation into each case and analyses the EOB claims. They enable appropriate decision-making and facilitate the required actions for recovery of dues.
Step 6 - Client Feedback
We evaluate the feedback shared by the client on data quality and make the necessary improvements and data quality refinements. This ensures the delivery of accurate and quality medical billing services.