 |
Medical Credentialing is the process of becoming affiliated with insurance companies so that you (the medical provider) can accept third party reimbursement.
Medical Enrollment process is a critical area of the program as it serves as the gateway for physicians and other health care providers into the program. Before physicians can bill Medicare they must submit an enrollment application to their Medicare contractor and have it successfully processed.
|
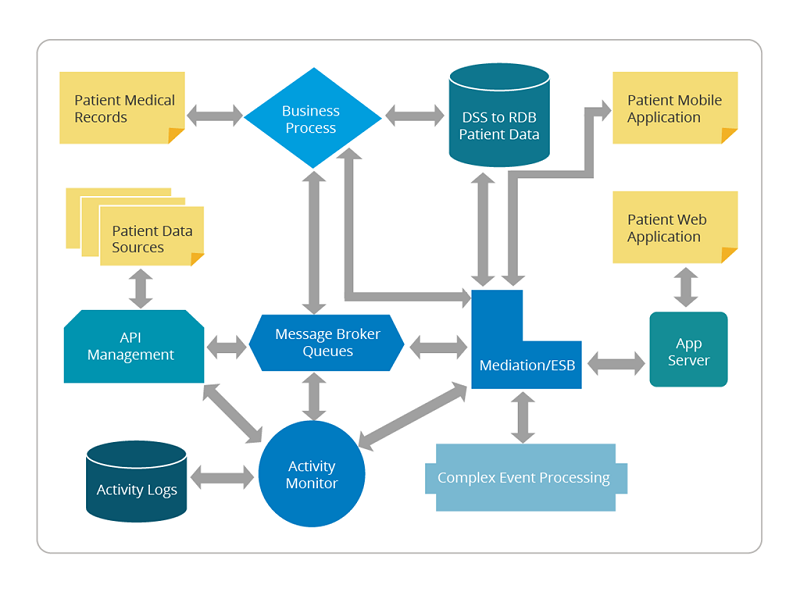
Enrollment Service
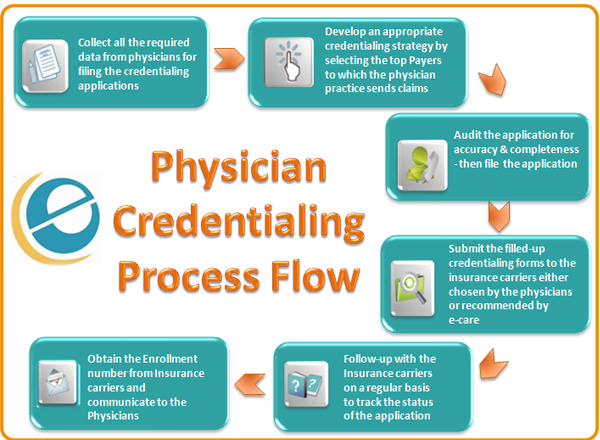
Credentialing Process Flow
Enrollment and credentialing services
Are you are starting your medical practice, moving on to a new one, looking to add new physicians to your group, or ensuring that your payments from insurer's health benefit claims do not get cancelled or rejected due to enrollment or credentialing issues? And is this tension eating up all your time and resources with little time left to focus on your practice?
If yes, all you need to do is, enrolling into expert enrollment and credentialing services and get contracted by insurers. Physician credentialing is invariably a tedious job, involving a lot of formalities and your valuable time as well, and with re-credentialing whenever needed it becomes even more annoying and deviation-bound, this is where relying on a professional service provider like its makes things easier and sensible.
SIDSOFT Pay Attention to your Enrollment & Credentialing Needs
Enrollment and credentialing services takes care of all your credentialing verification requirements like:
- Preparing necessary application forms and compiling all needed documents and certificates
- Verification of all the records and certificates
- Submission of all forms and documents, and ensuring faster approvals
- Taking care of all medical provider enrollment formalities and medical billing credentialing
- Preparing different forms based on the payer's or insurer's varied terms
- Maintaining each and every record necessary for the entire process
- Keeping track of expiration of NYS registrations, MA registrations, DEAs, and CLIA registrations and auto-handling re-applications for the same
- Processing re-credentialing whenever needed
Key Benefits SIDSOFT Deliver
We deliver the following key benefits to you through our healthcare credentialing services
- Hassle-free and faster payments from insurance companies
- Improved credibility among the insurance companies, helping in prompt and correct payments
- Steep reduction in accounts receivable days
- Improved customer satisfaction and increased goodwill, as a result of the process completed in a smooth and timely manner
- Ability to handle new clients using the same infrastructure
- Lots of time saved to focus on your patients
SIDSOFT Handles Medical Provider Credentialing Professionally
Medical credentialing specialists manage every client on a one-on-one basis. This ensures that all the enrollment and credentialing formalities are diligently addressed with faster processing and resolution of any enrollment or credentialing issues right from filing the applications to approvals. Our team also ensures that all applications are processed on a priority basis.
Leverage Advantage
- This is one of the leading enrollment credentialing, medical billing and medical transcription services company
- We employ exclusive specialists to handle key services
- This comes with globally appreciated quality assurance and trust